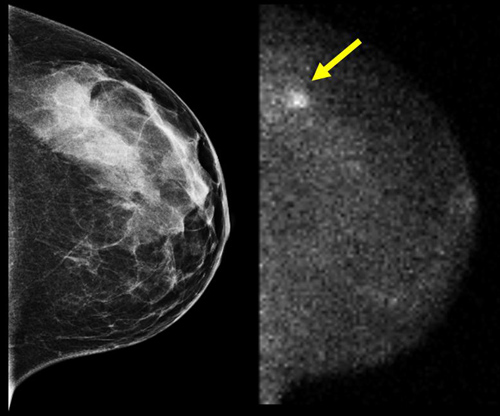
As dense breast tissue notification laws expand and draw media coverage, the role of molecular breast imaging (MBI) also is drawing more attention in breast cancer detection. New research looking at everything from lesion detection rates to specificity and dose reductions is helping breast imagers define MBI’s place in the rotation of adjunct breast imaging options.
Physicians and industry experts alike refer to a comparison between the functional imaging capabilities of MBI and the anatomical imaging aspects of other modalities when considering the benefits of pairing supplemental imaging with mammography. As MBI measures the metabolic activity of breast lesions by utilizing a radiotracer and a high-resolution gamma camera, users say this approach to breast cancer detection allows for more specific and efficient evaluation. MBI users also say this modality is more comfortable for the patient and comes with decreased costs and a reduction in the time necessary for physicians to interpret results.
“Functional imaging is the answer when looking at density,” says Jim Calandra, CEO of Gamma Medica, maker of the LumaGEM Molecular Breast Imaging System. “For example, when comparing the sensitivity of ultrasound, at 40% to 50%, to 80% to 90% sensitivity with MBI, it’s pretty clear that there’s a lot we’re not finding with ultrasound. You see more with MBI.”
While mammography remains the standard in breast cancer detection, sensitivity decreases in women with dense breast tissue. With more than one-half of women younger than age 50 and one-third of women older than age 50 diagnosed with heterogeneously dense or extremely dense breast tissue, physicians are looking for adjunct imaging to improve sensitivity in women with dense breast tissue. MRI has been a go-to modality for mammography follow-up in women with dense breast tissue due to its improved sensitivity, but MRI’s lower specificity increases false-positives that lead to more imaging and biopsies.
Gamma camera imaging brought with it the promise of greater specificity than MRI. As MBI technology evolves, researchers are improving their ability to gain the specificity improvement with less radiation exposure than a traditional gamma camera. As MBI technology evolves and patients receive less radiation during an exam, advocates believe its use may expand.
“MRI’s high sensitivity comes with low specificity, which leads to false-positives,” Calandra says. “There’s also cost, with MRI three to four times more expensive than MBI. Also, MRI is not an option for some women, as it can be intimidating, uncomfortable for women who are claustrophobic, and not viable for [many] women with pacemakers.”
MBI Research
The publication of new study results is helping to bolster the justification for including MBI modalities as adjuncts to mammography. Most recently, a retrospective study out of George Washington University reports that MBI is an effective adjunct imaging modality for detecting cancer regardless of breast tissue density. The study reviewed the cases of more than 300 patients with biopsy-proven breast cancer who underwent MBI. These patients had varying degrees of dense breast tissue or no density issues at all. MBI was found to have 95% sensitivity in women with and without dense breasts.
When looking at ultrasound as an adjunct to mammography in women with dense breast tissue, the researchers note that while it does increase sensitivity, it also substantially increases the false-positive rate.
The impact of dense breast tissue on various screening modalities is only one factor under consideration by a multi- disciplinary team of physicians at the Mayo Clinic in Rochester, Minnesota. Led by Michael K. O’Connor, PhD, FAAPM, a professor of medical physics in the department of radiology, the team is researching the newer-generation MBI equipment that allows for lower dose with no significant reduction of sensitivity. As early as 2011, the group found that low-dose MBI (reduced from the “label” recommended dose of 20 mCi to 8 mCi) is just as sensitive as conventional-dose MBI in detecting cancers missed by mammography in dense breast tissue.
And the dose is being reduced even further in the Mayo Clinic studies, where O’Connor says the researchers have gone as low as 6.5 mCi. That’s about one-third the dose used in earlier MBI studies, he says, and it greatly reduces radiation concerns surrounding MBI.
O’Connor also can envision a day when, with even lower dose numbers, MBI and mammography could have an even closer relationship. “At the Mayo Clinic, we’re using MBI for supple- mental screening,” he says. “With lower doses, we’d like to look at the possibility of doing an alternating schedule, with women having a mammogram one year and MBI the next year. We see this as a more practical approach that would be good for patients as well as help to lower health care costs.”
According to Robin Shermis, MD, MPH, medical director of ProMedica Breast Care in Toledo, Ohio, studies such as those under way at the Mayo Clinic confirm that radiation dose with MBI is not an issue for undue concern. “The old higher radiation dose and lower resolution of scintimammography in the past seem to have eliminated this option to many breast imagers,” he says. “The new low dose and imaging capabilities of MBI have completely changed the picture. We need to educate doctors and the public as to the true nature of radiation exposure with MBI. The worries of the past are just not justified.”
Workflow Considerations
Shermis, who also is a member of the Radiology Today editorial advisory board, refers to MBI as an ideal tool for “further screening women with dense breast tissue.” He has used Gamma Medica’s MBI technology for three years, completing more than 2,600 exams with this modality, and finds it to be easier to read and a quicker process than other modalities. “There is a learning curve,” he says, “but it’s pretty straightforward. There’s efficiency to reading MBI images. You can read them in real time, enabling you to provide patients with more immediate results and act on these results immediately. This also assists with workflow.”
Shermis’ center evaluates breast tissue density both subjectively and using the Volpara software to identify women who would benefit with additional screening beyond mammography.
Another consideration related to MBI dose issues is the amount of radiation the body actually absorbs. Jean Weigert,
MD, FACR, director of women’s imaging with The Hospital of Central Connecticut, has worked extensively with Dilon Diagnostics’ MBI system, which the company calls breast- specific gamma imaging (BSGI). “The dose [to the breast] is less than a mammogram, and the total body dose is less than that for a CT scan of the pelvis,” she says. “In the scheme of things, if you look at the global picture, this is insignificant.”
Weigert led a team that compared Dilon Technologies’ MBI/BSGI system with both mammography and ultrasound in patients who required further diagnostic imaging due to unclear clinical or radiographic findings. In a presentation Weigert gave at RSNA 2013, she noted that when comparing the sensitivity and specificity of mammography, ultrasound, and MBI/BSGI, “MBI/BSGI provided the highest independent sensitivity and when added to the diagnostic workup, MBI/ BSGI detected an additional 14 malignancies, increasing the sensitivity from 90% to 98%.”
According to Weigert, “A problem with screening ultrasound is that there are too many biopsies. You find so many things with ultrasound, but you don’t want to biopsy everything. We’ve been using MBI/BSGI on these types of cases. In patients with multiple areas of abnormality, you don’t know where to put the needle. MBI/BSGI helps with this.”
When it comes to comparisons with MRI, Weigert cites research showing greater specificity with MBI/BSGI. However, she also notes what you can and cannot see with MBI/BSGI. “You don’t see posterior tissue with MBI/BSGI, but for what you’re looking at [breast tissue], we’re not missing anything of concern,” she says. “If you’re looking at tissue outside the breast, you would use MRI. However, if the patient cannot have an MRI, then MBI/BSGI is a good alternative. You need to do the right test for the right person.”
Weigert also mentions benefits to recently released semi- quantitative analysis examining uptake concentrations and their relationship to how aggressive a cancer may be in that area.
The value in that uptake level relates to the woman’s cancer risk, she says. “This gives you some idea of how concerned you should be when you see areas of uptake,” Weigert says. “This is a good area to consider using a CAD [computer-aided detection] assessment tool to assess uptake.”
Dense Breasts, Otherwise Normal Risk
In Virginia, one state where radiologists are operating under breast density notification legislation, Jackson W. Kiser, MD, is turning to MBI as an adjunct to mammography, particularly as this demographic of women becomes more aware of the ramifications of dense breast tissue. He and James Crowley, BS, CNMT, molecular imaging and therapy supervisor, use the Dilon Molecular Imaging System with patients at LewisGale Regional Health System, part of HCA Virginia. Kiser says MBI use is good for women with dense breasts who have no other breast cancer risks; he considers it a routine screening tool in such women. He utilizes MRI in women with dense breast tissue who also have other high-risk factors, such as a family history of breast cancer.
“Now that women are receiving notifications, we can give them another weapon in the battle against breast cancer,” Kiser says. “In most cases, it’s economically more feasible to use MBI.”
In the days prior to MBI, Kiser says his team would use ultrasound to target a region in the breast where there was some question following mammography then biopsy the area. For tissue diagnosis, he says surgeons would rely on MRI for staging and to look at the patient’s lymph nodes.
Today, Crowley cites an example where utilizing MBI-guided breast biopsy enabled surgeons to pinpoint where to sample, allowing them to correctly identify that area as cancerous. “We see MBI as a great problem-solving tool,” Kiser says.
While breast imagers are figuring out how they prefer to use MBI, surgeons may be a tougher audience when it comes to discussions regarding the benefits of MBI. Both Kiser and Crowley say that surgeons are used to pure anatomical studies rather than functional imaging studies that show metabolic activity associated with cancerous lesions. Kiser says that not all surgeons can conceptualize the view obtained via MBI modalities. “Physicians are taught to read anatomic views in medical school,” Crowley says. “Functional imaging is not taught.”
Another potential advantage to MBI’s adoption is the financial impact of purchasing, running, and maintaining new equipment in the current economy and uncertainty created by the Afford- able Care Act. When compared with other modalities, Shermis says MBI is the most cost-effective adjunct to mammography. MRI is more expensive, and ultrasound is a high resource drain.
“We use MRI at our center for high-risk women with dense tissue and MBI for women who have a dense mammogram that are not at high risk or who cannot have an MRI,” he says. “MBI is not that expensive. It has lower reimbursement than MRI, but it’s an efficient modality for breast cancer detection. It’s not expensive to purchase or to perform, and it’s efficient to read.”
Health Care Influencers
With the focus on women’s health care, Calandra says offering MBI can give hospitals an advantage in the marketplace.
He sees women driving many family health care decisions, and hospitals and breast imaging centers are making equipment purchase decisions with that in mind. “Women’s health is an important element of the health care systems we work with,” he says. “In many cases, women are making decisions for the entire family. When it comes to their own health care needs, they’re choosing to go to the centers where they can get the best services. They’re making medical decisions based on where they can get the best care possible.”
Part of the decision to offer MBI includes where this modality can fit into an existing practice workflow. Unlike MRI, Calandra notes that an MBI system does not require construction of a separate facility and is configured in a manner that users are familiar with. “Workflow is no more complicated than going from mammography to ultrasound or mammography to MRI,” he says.
With several studies and clinical trials under way, the goal for radiologists and physicians working in breast imaging is to find what works best, understanding that there may not be just one answer to that question. “It’s about finding the right mix for each situation,” Weigert says.
— Kathy Hardy is a freelance writer based in Phoenixville, Pennsylvania. She writes primarily about women’s imaging issues for Radiology Today.